Your Stories: Saint Francis Perioperative Team Attends Continuing Education Seminar
July 15, 2024Categories: Colleague Corner
 Saint Francis Hospital Perioperative nurses and surgical techs recently attended a Continuing Education (CE) in person lecture to learn about the risks of insufflation pressure for patients during laparoscopic and robotic abdominal surgery and the benefits of utilizing low insufflation pressure.
Saint Francis Hospital Perioperative nurses and surgical techs recently attended a Continuing Education (CE) in person lecture to learn about the risks of insufflation pressure for patients during laparoscopic and robotic abdominal surgery and the benefits of utilizing low insufflation pressure.
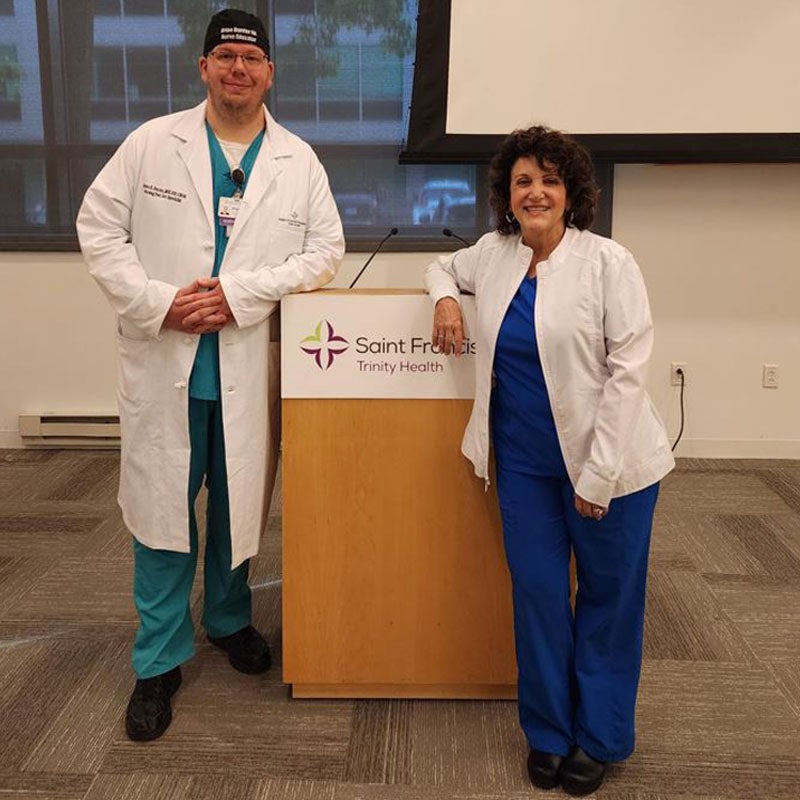
Vangie Dennis, MSN, RN, CNOR, CMLSO, a Perioperative Nurse Consultant with a long history of advocating for Perioperative staff and patients, came to Saint Francis to present the live lecture. Vangie is a previous president of the Association of Perioperative Registered Nurses (AORN) and has a strong commitment around Perioperative nursing leadership and education. Vangie’s passions lie in educating staff with topics such as smoke evacuation, insufflation, and laser safety. Vangie is an engaging speaker and the Saint Francis team felt lucky to have her at the hospital to present in person.
The education comes at a critical time, as in today’s surgical world, patients are undergoing more minimally invasive surgical procedures than ever before. While these procedures certainly have their advantages over traditional “open” incision surgery, there are new, unique risks involved. Introducing CO2 gas into the abdomen for the purpose of abdominal distention is the process of achieving pneumoperitoneum by insufflation. This insufflation pressure must be maintained in order for the surgeon to operate within the abdominal cavity. However, there are several risks presented to patients under insufflation, including causing pressure on vital organs, minimizing venous blood flow return, and the possibility of an embolism. Furthermore, there is also general pain and discomfort felt by patients post operatively. Studies have shown that patients have less discomfort and pain and achieve better outcomes after low insufflation pressure has been utilized. Patients with less pain require less pain management and recover safer and faster, meaning they can potentially leave the hospital faster as well.
Low pressure insufflation technology has been a staple of robotic surgery for a long time. However, there is a shift in the surgical world, where low pressure insufflation is desired in all laparoscopic surgery as well. High acuity patients with multiple co-morbidities and obese patients benefit the most from low pressure stable pneumoperitoneum. When Saint Francis converted to smoke evacuation in January, the team also introduced the new insufflator technology in all of the operating rooms to be used laparoscopically and during robotic surgeries. The bariatric surgical team prefers to utilize low pressure insufflation for safer surgery and better patient outcomes.
“Our colleagues are always asking for engaging, live, in person CE opportunities, and some of our staff require education credits for certifications and licensing,” said Brian Burrier, MSN, RN, CNOR, Nursing Professional Development Specialist. “It was an absolute pleasure to be able to coordinate and bring this amazing education to my OR staff. The lecture was very engaging, and everyone learned a lot about insufflation safety. Saint Francis is dedicated to our value of patient safety, and I am grateful I get the opportunity to bring this amazing education to our staff to keep all our patients safe every day!”
Submitted by Brian K. Burrier, MSN, RN, CNOR, Nursing Professional Development Specialist, Saint Francis Hospital.
Have a story you want to share? Submit your story at TrinityHealthOfNE.org/YourStories
